Many people have never heard of celiac artery stenosis until they start experiencing unexplained abdominal pain or digestive issues. It’s a condition that involves the narrowing of the celiac artery—a major blood vessel supplying blood to your stomach, liver, and other organs. While it may sound rare or even harmless at first, many begin to wonder, is celiac artery stenosis dangerous?
The short answer is—it can be. But not always. Some people live with it for years without even knowing. For others, it causes life-disrupting symptoms that need medical attention. The level of danger depends on the severity, underlying cause, and how your body reacts to the reduced blood flow. This article will break down what you need to know about celiac artery stenosis, from symptoms to treatment, so you can make informed decisions about your health.
What Is Celiac Artery Stenosis?
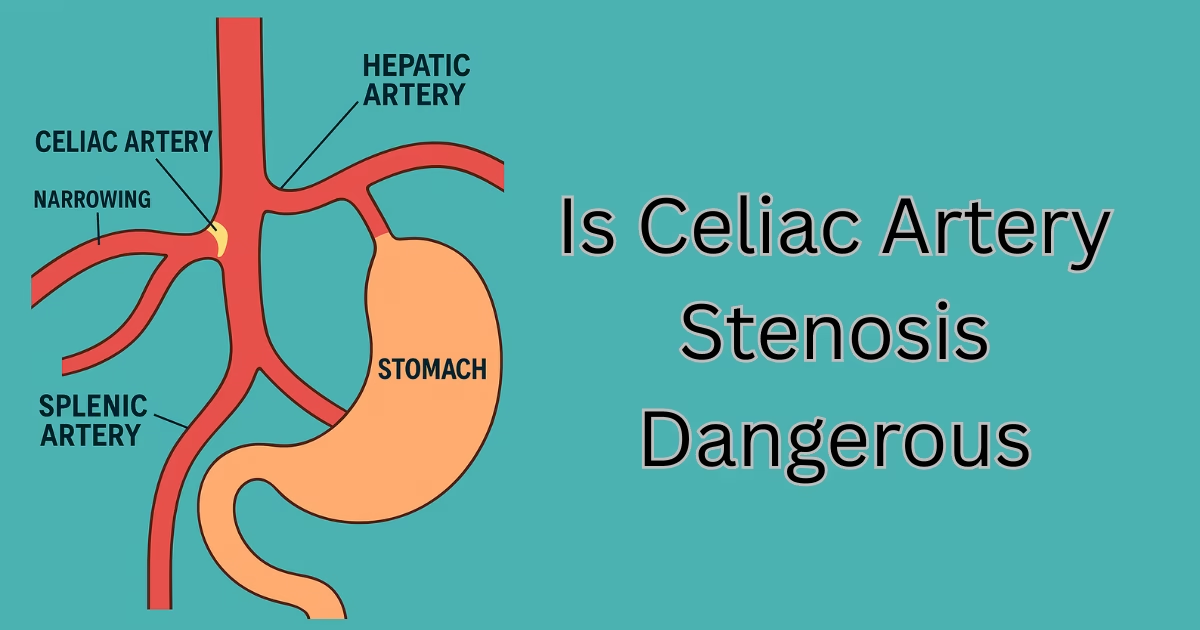
Celiac artery stenosis is a condition where the celiac artery becomes narrowed or compressed. This artery branches off the aorta and is responsible for supplying blood to some of your most important digestive organs—including the liver, stomach, and spleen.
In a healthy person, blood flows freely through this artery. But when stenosis (narrowing) happens, that flow gets restricted. The most common reasons for this include plaque buildup (atherosclerosis) or an anatomical issue like median arcuate ligament syndrome (MALS), where a ligament presses on the artery.
People of any age can be affected, but it’s more common in older adults and those with heart disease risk factors. The condition may go unnoticed in many, especially if it’s mild. But in others, it can cause serious symptoms that affect daily life and digestion. Understanding the basics is the first step toward recognizing whether treatment is needed.
Is Celiac Artery Stenosis Dangerous?
This is the big question. Is celiac artery stenosis dangerous?
The answer depends on a few things—how narrow the artery is, what’s causing it, and how your body is handling the reduced blood flow. If your organs are still getting enough blood, it might not be dangerous right away. You might not feel any symptoms, and your doctor could even miss it on routine checkups.
But when the narrowing is severe, it’s a different story. Without enough blood, your stomach and intestines may not work right. This can lead to pain, weight loss, and trouble digesting food. In rare cases, serious damage to your organs can happen over time.
There’s also a risk that the blockage could worsen, especially if it’s caused by atherosclerosis. That raises the chance of developing chronic mesenteric ischemia—a condition where blood flow to the gut is so low that tissue starts dying.
So yes, celiac artery stenosis can be dangerous, especially if ignored.
Symptoms You Shouldn’t Ignore
The tricky part is that symptoms can be mild or vague. Some people don’t even know they have this condition until it gets worse. Still, there are signs you should never brush off.
One of the most common symptoms is pain in the upper abdomen, especially after eating. This happens because your organs need more blood during digestion, and a narrowed artery just can’t keep up.
Other signs may include:
- Nausea or vomiting
- Feeling full quickly when eating
- Unexplained weight loss
- Diarrhea or changes in bowel habits
- Fatigue after meals
Some describe the pain as dull and cramping, others feel sharp or stabbing. It varies. If you notice a pattern—like pain that comes after eating and gets better when you skip meals—it’s worth talking to a doctor.
Causes and Risk Factors
Understanding what causes celiac artery stenosis can help you manage it better.
Here are the common causes:
- Atherosclerosis: Plaque buildup from cholesterol hardens and narrows the artery.
- MALS (Median Arcuate Ligament Syndrome): A ligament compresses the celiac artery.
- Fibromuscular dysplasia: Abnormal growth of artery walls.
- Blood clots or tumors (less common but possible)
And here are risk factors that can increase your chances:
- Age over 50
- High cholesterol
- Smoking
- Diabetes
- High blood pressure
- Family history of vascular diseases
Also, some people are born with anatomy that makes them more likely to develop compression of the celiac artery. It’s not always related to lifestyle.
How It’s Diagnosed
Getting the right diagnosis is key. Many people go through several tests before doctors figure out what’s wrong.
Here are the most common ways it’s diagnosed:
- CT Angiography: Gives a detailed image of blood flow and artery shape
- Doppler Ultrasound: Measures blood flow through the celiac artery
- MR Angiography (MRA): A type of MRI that looks at blood vessels
- Catheter Angiography: An invasive test, but very accurate
Sometimes, doctors test blood flow while you’re breathing in and out to see if a ligament is compressing the artery—useful in diagnosing MALS.
Misdiagnosis happens, especially if doctors mistake it for acid reflux or gallbladder problems. So if your symptoms don’t go away, don’t give up. Ask for a second opinion.
Treatment Options Available
If your case is mild and you’re not having symptoms, you might not need treatment right away. But if you’re in pain or losing weight, treatment becomes important.
Here are the main treatment paths:
Lifestyle Changes:
- Eating smaller meals more often
- Avoiding high-fat foods
- Managing blood pressure and cholesterol
- Quitting smoking
Medications:
- Blood thinners (if clots are a concern)
- Cholesterol-lowering drugs
- Pain management (temporary relief only)
Surgery:
- Angioplasty and Stenting: Opens the artery and places a stent to keep it open
- Bypass Surgery: Creates a new route for blood flow
- Ligament Release (for MALS): Relieves pressure from the artery
Surgery isn’t for everyone, but it can help those with severe symptoms. Recovery time varies, but most patients feel better within weeks.
Living with Celiac Artery Stenosis
Yes, you can live a normal life with this condition—especially if it’s caught early.
If symptoms are managed and you follow your doctor’s advice, many people feel well enough to return to normal routines. It’s about making smart choices and paying attention to your body.
Here are a few daily tips:
- Eat slowly and chew well
- Don’t skip meals, but don’t overeat
- Stay active with light exercise
- Keep regular appointments for checkups
Even after treatment, follow-up is important. Arteries can narrow again over time, especially if you have risk factors like high cholesterol or diabetes.
When to See a Doctor
Don’t wait too long if you notice signs like:
- Pain after meals
- Weight loss without trying
- Feeling full too quickly
- Nausea that keeps coming back
These could point to more than just an upset stomach. The earlier you catch it, the better your chances of avoiding long-term damage.
If you’ve already been diagnosed, watch for any changes in symptoms. And if your pain gets worse or new symptoms appear, seek medical help right away.
It’s better to be safe than sorry when blood flow to your organs is involved.
Also Read: Diseases Similar to Celiac Disease: Causes, Symptoms, and Diagnosis
Conclusion
So, is celiac artery stenosis dangerous? The truth is, it can be—especially if it’s ignored or left untreated. But with early diagnosis and proper care, most people can manage it well and live a healthy life.
Understanding the symptoms, knowing the risks, and talking to a doctor if anything feels off can make all the difference. Whether it’s caused by plaque, MALS, or something else, don’t brush it off. You only get one set of digestive organs, and they need proper blood flow to do their job.
If you’ve been wondering about that nagging pain after meals, it might be time to ask the right questions. Don’t wait until it gets serious.
FAQs About Celiac Artery Stenosis
1. What is the main cause of celiac artery stenosis?
The main cause is usually atherosclerosis, which is the buildup of plaque in the artery. In some cases, it’s due to median arcuate ligament syndrome (MALS).
2. Is celiac artery stenosis life-threatening?
It can be if left untreated, especially in severe cases where blood flow is reduced enough to damage organs.
3. Can celiac artery stenosis go away on its own?
No, it doesn’t go away on its own. Mild cases might not need treatment right away, but monitoring is important.
4. What are the first signs of celiac artery stenosis?
Common early symptoms include upper abdominal pain after eating, nausea, and unintentional weight loss.
5. How is celiac artery stenosis treated?
Treatment may include lifestyle changes, medications, or surgery such as angioplasty, stenting, or ligament release (in MALS cases).