The celiac ganglion is a vital component of the autonomic nervous system, playing a significant role in regulating several important functions within the body. Located in the abdomen, it serves as a key player in controlling the digestive process by influencing various abdominal organs, including the stomach, liver, pancreas, and intestines. The celiac ganglion is part of the sympathetic nervous system, which is responsible for the body’s “fight or flight” responses, but it also plays a crucial role in maintaining everyday bodily functions. Understanding the celiac ganglion and its functions is essential for gaining insight into how our body manages digestion, metabolism, and pain. This article explores the anatomy, function, and clinical relevance of the celiac ganglion, providing a comprehensive overview of its importance in both health and disease.
What is the Celiac Ganglion?
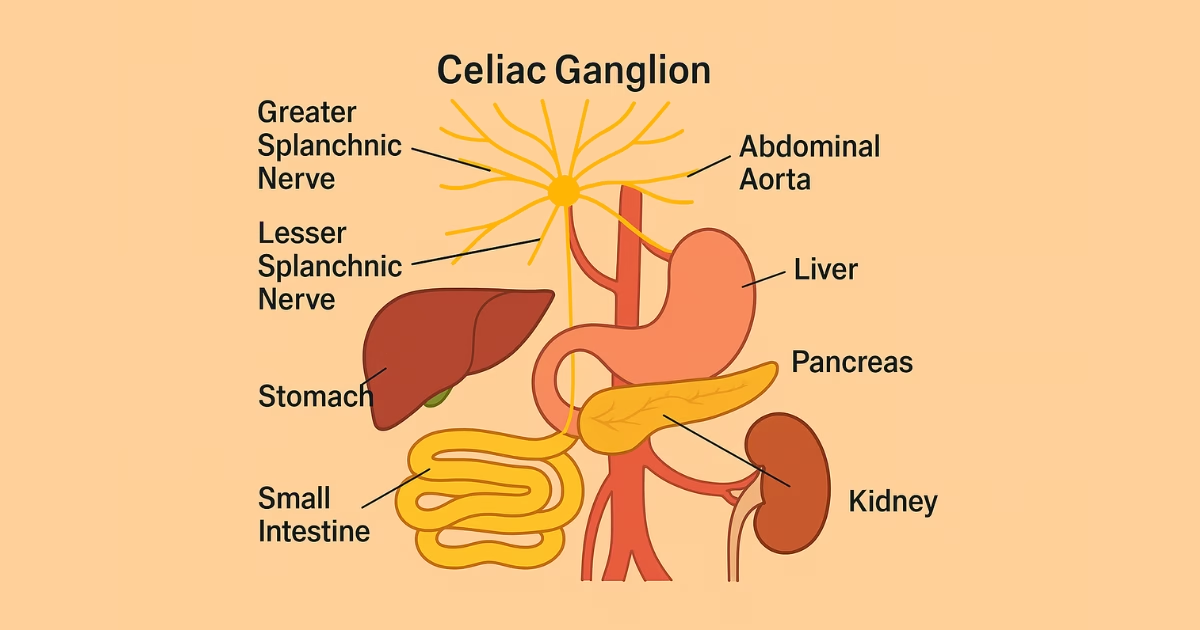
The celiac ganglion is a large, dense nerve cluster located in the upper abdomen, near the origin of the celiac artery. It is one of the major ganglia in the sympathetic nervous system and plays an essential role in regulating the body’s digestive processes. This ganglion acts as a relay station for nerve signals, sending and receiving messages from the brain to various abdominal organs, including the stomach, liver, pancreas, and intestines.
Anatomically, the celiac ganglion is situated behind the stomach and in front of the aorta, just below the diaphragm. It is connected to other sympathetic nerves, which help control involuntary body functions. These include processes such as the secretion of digestive enzymes, the movement of food through the digestive tract, and the regulation of blood flow to digestive organs.
The celiac ganglion is closely linked to the celiac plexus, a network of nerves that further expands its reach to organs throughout the abdomen. This connection is critical for coordinating the proper functioning of the digestive and metabolic systems.
The Functions of the Celiac Ganglion
The celiac ganglion plays a critical role in the autonomic regulation of the body’s digestive processes. As part of the sympathetic nervous system, it helps control various physiological functions in the abdomen. One of its primary responsibilities is regulating the flow of signals between the brain and key abdominal organs such as the stomach, liver, pancreas, and intestines.
Autonomic Control: The celiac ganglion regulates autonomic functions, which are involuntary processes that keep the body functioning without conscious effort. These include the secretion of digestive enzymes and gastric juices, as well as the motility (movement) of food through the digestive tract. The ganglion works to balance these functions during both rest and periods of stress.
Digestive Regulation: The celiac ganglion directly influences digestion by controlling the smooth muscle of the stomach and intestines. It ensures that digestive processes, such as the breakdown and absorption of nutrients, occur efficiently. The celiac ganglion also helps coordinate the release of insulin and other hormones from the pancreas, which play a role in regulating blood sugar levels and metabolism.
Metabolic Functions: The ganglion is involved in regulating liver functions as well. It helps manage bile production, which is essential for fat digestion. Additionally, it plays a role in glucose metabolism, ensuring that the body maintains an appropriate balance of energy.
Blood Flow Management: The celiac ganglion also helps regulate the blood flow to various abdominal organs. By controlling the dilation and constriction of blood vessels, it ensures that organs like the liver and intestines receive the appropriate amount of blood during digestion, particularly when food is being processed.
Clinical Significance of the Celiac Ganglion
The celiac ganglion has clinical significance, especially in the treatment of certain abdominal conditions. It has become a target for medical interventions, particularly for chronic pain relief and for patients dealing with digestive system disorders.
Celiac Plexus Block: One of the most well-known procedures involving the celiac ganglion is the celiac plexus block. This procedure involves injecting local anesthetics or other medications around the celiac plexus to block nerve signals. It is used as a treatment for patients suffering from chronic abdominal pain, especially those with conditions like pancreatic cancer, chronic pancreatitis, or other gastrointestinal disorders. The celiac plexus block can offer significant relief for individuals experiencing severe, persistent pain.
Impact on Abdominal Pain: The celiac ganglion plays an essential role in transmitting pain signals from the abdominal organs. When there are dysfunctions in the ganglion, it can lead to conditions like visceral pain syndromes, which can cause chronic, unexplained abdominal pain. By addressing issues in the celiac ganglion, doctors can help alleviate these painful symptoms, offering a better quality of life for patients.
Role in Pain Management: The celiac ganglion’s role in pain transmission has made it a focus of research in pain management. For example, celiac ganglion ablation, which involves destroying nerve tissue, may be performed in certain cases where the celiac plexus block is ineffective. These procedures aim to disrupt the transmission of pain signals, helping to manage and control chronic pain related to abdominal diseases.
Disorders Linked to Celiac Ganglion Dysfunction
Dysfunction in the celiac ganglion can lead to several health issues, most notably related to digestive and abdominal pain. When the ganglion fails to function properly, it can cause disruptions in the nervous control of abdominal organs, leading to a range of symptoms.
Visceral Pain Syndromes: One of the most common outcomes of celiac ganglion dysfunction is visceral pain, a form of pain originating from internal organs. This pain may be felt in the abdomen, but it can also radiate to other parts of the body. Dysfunction of the celiac ganglion can disrupt the proper transmission of pain signals from abdominal organs to the brain, leading to chronic discomfort.
Autonomic Dysfunction: Since the celiac ganglion is part of the autonomic nervous system, damage to it can lead to broader autonomic dysfunctions. This can affect the regulation of digestion, metabolism, and heart rate. For example, conditions such as irritable bowel syndrome (IBS), gastrointestinal motility disorders, or gastroparesis may be linked to disturbances in the celiac ganglion’s function.
Symptoms of Dysfunction: Common symptoms associated with celiac ganglion dysfunction include chronic abdominal pain, bloating, nausea, and changes in appetite or digestion. Additionally, patients may experience unexplainable weight loss or malabsorption, which can result from the ganglion’s inability to properly regulate digestive processes.
Surgical and Non-Surgical Treatments Involving the Celiac Ganglion
There are both surgical and non-surgical treatment options available for addressing conditions associated with the celiac ganglion, especially in cases of chronic abdominal pain or dysfunction.
Surgical Procedures: In some cases, surgical procedures are necessary to address issues with the celiac ganglion. For instance, splanchnicectomy is a surgery in which part of the sympathetic nerve fibers around the celiac ganglion are removed or interrupted. This can help alleviate chronic abdominal pain in certain patients, particularly those with cancer or other persistent conditions.
Non-Surgical Interventions: Celiac plexus blocks are a less invasive treatment that involves injecting medication directly into the celiac plexus. This can provide significant relief for patients with pain associated with abdominal organs. Other treatments, such as nerve ablation or the use of specialized medications to regulate nerve function, may also be used to help manage symptoms.
Recovery and Risks: The risks associated with these treatments vary depending on the procedure. While celiac plexus blocks have a relatively low risk of complications, surgical interventions like splanchnicectomy carry a higher risk due to their invasive nature. Recovery times differ, but most patients can expect to experience some improvement in symptoms after undergoing these treatments.
The Role of the Celiac Ganglion in Modern Medicine
The celiac ganglion has become a focus of modern medical research, particularly in the areas of pain management, digestive health, and the treatment of chronic abdominal conditions. As scientists continue to explore its functions and clinical applications, new treatments are being developed to harness the ganglion’s role in the autonomic nervous system.
Research and Advancements: Medical research is increasingly focusing on understanding how the celiac ganglion and its associated plexus can be manipulated to improve patient outcomes. Techniques like nerve blocks and ablations are becoming more refined, offering targeted relief for patients suffering from pain. There is also growing interest in understanding how the celiac ganglion affects overall metabolic processes, which could lead to new treatments for conditions like diabetes or obesity.
Future Directions: The future of celiac ganglion-related research holds promising possibilities. As technology advances, it may become possible to develop more precise, non-invasive techniques for addressing celiac ganglion dysfunction. Additionally, better understanding of its role in metabolic health could lead to innovative therapies for treating various chronic conditions, further improving the quality of life for many patients.
Also Read: Can Celiac Disease Cause Hemorrhoids? Symptoms & Risks Explained
Conclusion
In conclusion, the celiac ganglion is an essential part of the autonomic nervous system, playing a crucial role in regulating the digestive processes, metabolism, and pain management. Whether through its influence on the stomach, liver, pancreas, or intestines, the celiac ganglion is a key player in maintaining bodily functions that we often take for granted. Understanding its function is not only critical for medical professionals but also for patients dealing with abdominal pain, digestive disorders, and metabolic issues. By exploring both its normal functions and its role in disease, we can continue to develop effective treatments that improve patient outcomes. Whether through non-surgical interventions or advanced research, the celiac ganglion remains a critical focus in modern medicine.

Hi, I’m Shafy Ali – a curious mind and passionate writer at Celiac Magazine. I cover a little bit of everything, from everyday tips and how-tos to deeper dives into topics that spark conversation. I enjoy turning research into readable, relatable content that informs and inspires. Whatever the subject, I aim to keep it clear, engaging, and genuinely useful.